The cause of hypercoagulopathy with COVID-19 may be due to autoantibodies, new study shows, creating potential for increased demand for autoantibody testing
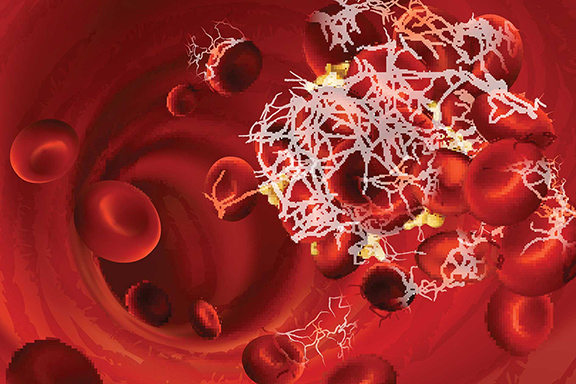
Since the early days of the COVID-19 pandemic, researchers recognized hypercoagulopathy as a significant complication of COVID-19. Initially, the cause of COVID-19-associated hypercoagulopathy was not well understood, but the complication persisted to become a major risk factor for both hospitalization and mortality rates.
 Pulmonary embolisms are common in patients who have severe or critical cases of COVID-19. The COVID-19 STAT Intelligence Briefings Service reported on this complication in late July 2020. At that time, we spoke with Joshua Hayden, PhD, DABCC, FAACC, Chief of Chemistry for Norton Healthcare, about certain laboratory tests for hypercoagulopathy, that clinical laboratories were overlooking.
Pulmonary embolisms are common in patients who have severe or critical cases of COVID-19. The COVID-19 STAT Intelligence Briefings Service reported on this complication in late July 2020. At that time, we spoke with Joshua Hayden, PhD, DABCC, FAACC, Chief of Chemistry for Norton Healthcare, about certain laboratory tests for hypercoagulopathy, that clinical laboratories were overlooking.
When COVID-19 STAT spoke with Hayden, understanding hypercoagulopathy in COVID-19 was still in its infancy. At the time, Hayden referred to hypercoagulopathy as “a question mark” for follow-up and discussed the potential importance of certain types of potentially appropriate clinical laboratory testing related to COVID-19 outcomes. (See Clinical Laboratories May be Overlooking Coagulopathy Tests That Should Be Ordered for COVID-19 Positive Patients.)
University of Michigan Team Explores Hypercoagulopathy With COVID-19
Now, the medical community’s knowledge of the cause of COVID-19-related hypercoagulopathy benefits from new research published in early November 2020. The new findings come from a team of researchers at the University of Michigan, who have published a paper in Science discussing that a specific set of autoantibodies attack blood vessel cells, leading to excessive clotting in patients with COVID-19.
The autoantibodies that were discovered to be responsible for this effect—aPL antibodies—are the same antibodies that are responsible for antiphospholipid syndrome, a potentially life-threatening thrombophilia. With this condition, patients develop pathogenic autoantibodies that target phospholipids and phospholipid-binding proteins.

Yogen Kanthi, MD, Assistant Professor at the University of Michigan and one of the paper’s authors said, in a recent interview, that COVID-19 can be seen as “an extreme version of a number of diseases, one of them being antiphospholipid syndrome. We knew antibodies like this can exist but no one ever looked to see if they can cause clotting,” Kanthi said.
Insights into the Mechanisms Behind the Pathology of COVID-19 Coagulopathy
These recent findings provide deeper insights into the mechanisms behind the pathology of COVID-19-related coagulopathy. “I think that so much attention in COVID has been spent on diagnosis and not really understanding what patients need—increased management and attention,” Hayden had told COVID-19 STAT when research in this area had not yet revealed these new findings. “The question is how do you catch those people who are suffering serious life-threatening complications and have more severe cases?”
With these new findings, new ways of detecting serious cases of COVID-19 may soon be possible. The findings of the team from the University of Michigan seem to indicate that testing for aPL antibodies could help to predict the hypercoagulopathy that sometimes accompanies COVID-19. While these findings are new, clinical laboratory directors should stay apprised of developments in this area.
Clinical laboratories may also benefit now from considering the possibility of increased demand for testing aPL antibodies. By preparing for this potential demand now, clinical laboratories may be better positioned to accommodate increased demand in this area as research continues.

—By Caleb Williams, Editor, COVID-19 STAT
Related Resources:
Yahoo News: Scientists Have Uncovered the Likely Cause of a Serious COVID-19 Symptom: Blood Clotting
Frontiers in Immunology: Cardiac Manifestations of Antiphospholipid Syndrome With Focus on Its Primary Form