Norton Healthcare chief of chemistry points out shortcomings in post-diagnostic laboratory studies for COVID-19 positive patients.
As clinical laboratories around the country focus on testing patients for COVID-19 and ensuring that they can provide diagnostic testing, some laboratories may be overlooking tests that should be ordered to follow up once a COVID-19 positive patient is identified.
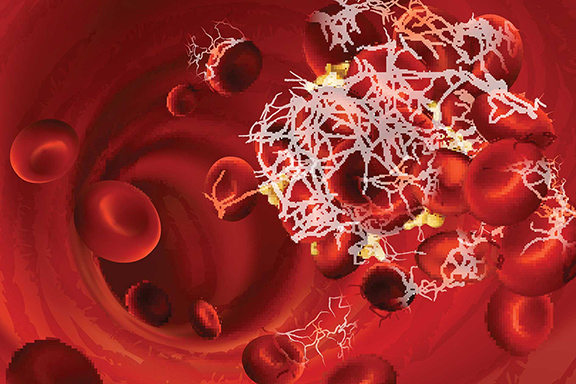
The growing body of evidence about the pathology of COVID-19 has indicated that the course of a severe COVID-19 infection involves coagulopathy that can have devastating consequences. A recent study published in Radiology: Cardiothoracic Imaging found that over 37% of patients who were positive for COVID-19 in an ICU setting were found to have a pulmonary embolism (PE) on computed tomography pulmonary angiogram (CTPA).
To better understand the coagulopathy caused by COVID-19 and how clinical laboratories should be approaching this complication, the COVID-19 STAT Intelligence Briefings Service spoke with Joshua Hayden, PhD, DABCC, FAACC. Hayden is Chief of Chemistry for Norton Healthcare, and previously served as Assistant Professor of Pathology and Laboratory Medicine at Weill Cornell Medical College.
COVID-19 and Coagulopathy

Chief of Chemistry for Norton Healthcare Joshua Hayden, PhD, DABCC, FAACC (above), discussed the potential importance of certain types of follow-up clinical laboratory testing related to COVID-19 outcomes. (Photo used with permission.)
Hayden discussed with STAT COVID-19 the pathology of how COVID-19 associated coagulopathy is caused. “There still is a lot we have to learn. My understanding of the underlying mechanism is that increased vascular permeability causes exposure and activation of the clotting factors,” Hayden explained. “Certainly we’ve seen it with the inflammatory markers like IL6 which we know from just a basic physiology standpoint can be involved in that whole process. So it seems likely that that is contributing to this sort of coagulopathy.”
Hayden cautioned that there are still several unknowns. “Just because a story seems to make sense and seems plausible it doesn’t mean that it’s by any means proven,” Hayden said. “And whether there’s something else going on there or not I think is still a question mark and something that I think will need to be followed up.”
Hayden offered insights into how clinical laboratories should be thinking about COVID-19 positive results. “I think something that we’ve been very interested in in our health systems is the idea of really going beyond diagnosing,” Hayden explained. “So many times when we talk about testing for COVID-19, we think about the PCR, and really we know that the majority are going to be asymptomatic or have very mild symptoms. The question is how do you catch those people who are suffering serious life-threatening complications and have more severe cases?”
About the Importance of Utilizing D-dimer to Rule Out PE in COVID-19 Positive Patients
While Hayden explained that the science is still being studied, he suggested laboratory tests that should be considered for COVID-19 positive patients. “I do think that within the limits of our knowledge so far, it seems reasonable to suspect that D-dimer is going to have a very high negative predictive value [for ruling out PEs],” Hayden explained. “They are saying there’s no need for additional studies for PEs. With the evidence that we have so far, I think it would be reasonable standard of care to utilize D-dimer to rule out PE in these COVID-19 patients, but whether that’s actually supported by studies in this patient population is not entirely clear.”
A Potential Clinical Laboratory Testing Strategy
Other laboratory tests should be performed when considering the coagulopathy that COVID-19 may cause., according to Hayden. “Moving beyond the PE, just looking at the coagulopathy, in our health system we’re looking at D-dimer levels, but we’re also getting daily fibrinogens and daily [partial thromboplastin time] PTT levels. Those additional coag markers are going to be helpful looking for that consumptive DIC-type picture.”
The primary clinical advantage to considering these additional laboratory tests, according to Hayden, is that it allows the most efficient allocation of resources where they are needed most. “We have found some of these laboratory markers useful for triaging patients and saying ‘this patient is very sick, the odds of them having an adverse outcome due to the disease is exceedingly high, and therefore whatever risk is associated with this therapeutic is probably worth the potential reward.’”
Clinical laboratory directors may be able to increase test volumes by bringing attention to, and developing protocols for, coagulopathy testing for COVID-19 positive patients, including D-dimers, PTTs, and fibrinogen. Hayden told STAT COVID-19, “I think that so much attention in COVID has been spent on diagnosis and not really understanding what patients need—increased management and attention.” By bringing attention to post-diagnostic testing, laboratories can better serve COVID-19 positive patients.

—By Caleb Williams, Editor, COVID-19 STAT
Related Resource:
Radiology – Cardiothoracic Imaging: Pulmonary Embolism on CTPA in COVID-19 Patients