A retrospective look at three COVID-19 testing trends impacting clinical laboratories
At the beginning of 2020 no one could have predicted the unusual and impactful year that would follow. The COVID-19 pandemic not only created widespread changes to public behaviors but also led to a constantly changing clinical landscape for clinical laboratories to navigate.
The COVID-19 STAT Intelligence Briefings Service has closely followed changes and trends that affect clinical laboratories, keeping the nation’s top laboratories apprised of changes as, or before, they occur. While COVID-19 related changes have been varied and numerous, we review some of the more significant COVID-19 trends of 2020 as the year has drawn to a close.
1. Rapid, Point-of-Care Testing for Coronavirus
In the early days of the COVID-19 pandemic, clinical laboratories were testing for SARS-CoV-2 using almost exclusively RT-PCR-based tests. These genetic tests were highly sensitive and specific, but they failed to offer the quick turnaround times that local governments, businesses, and academic institutions felt were necessary. The time that it took to send specimens to a laboratory and get the results back was typically 24-48 hours. The timeframe was often longer due to the supply chain shortages that clinical laboratories continue to face.
Having a test that could be performed and resulted quickly, especially at the point of care (POC), became recognized as an important part of reopening during the pandemic. The demand for these tests soared as lockdowns started to end. Antigen testing offered the earliest opportunities for rapid testing and could be performed at the point of care, making results possible within minutes, not days. While these tests were known to provide higher rates of false positives than PCR testing, the rapid results that antigen testing offer helped them to gain significant public and political attention over the summer as lockdowns ended.
Antigen testing became more prominent in July 2020. In early July, BD (Becton, Dickinson and Company) received an emergency use authorization (EUA) for its antigen test (See Antigen SARS-CoV-2 Diagnostic Test EUA Update), making two antigen tests available for the public. Mid- to late-July saw significant investment by the federal government into antigen testing. Publicly funded antigen tests were made available to most nursing homes in the United States by the end of the month (See HHS Invests $24 Million Into Scaling the Production and Accessibility of POC SARS-CoV-2 Antigen Tests, Reducing Need for Clinical Lab Based Tests).
In early August, a group of seven states signed an agreement to purchase 500,000 antigen tests each and, by the end of the month, another antigen test by Abbott had been authorized. The federal government inked a $750 million deal with Abbott within 48 hours (See Abbott SARS-CoV-2 Antigen Test Receives EUA, Had $750 Million Deal Pending With Federal Government in Less Than 48 Hours). Other countries began relying heavily on antigen testing. The Netherlands became the first country to order antigen tests at a national level, with an order for 9.2 million tests in early November (See Demand for SARS-CoV-2 Antigen Tests Shows No Signs of Slowing as Netherlands Orders 9.2 Million Tests from BD).
While the initial enthusiasm for antigen testing was strong, problems emerged. The false-positive rate, especially in low-prevalence areas, created difficulties and inconveniences that caused some institutions to stop using antigen testing altogether. The US Department of Health and Human Services (HHS) recognized this problem and, in late November, launched a pilot program examining the possibility of integrating POC genetic testing into existing antigen testing models (See HHS Launches Pilot Program Examining the Use of Integrating Rapid Molecular COVID-19 Test Into Existing Testing Strategies).
2. At-Home and Nonprescription COVID-19 Tests
While antigen testing dominated the competition that clinical laboratories faced for COVID-19 testing, another trend became even more concerning as a source of potential competition by the end of 2020. COVID-19 testing is moving out of the realm of clinical laboratories, and some tests may no longer require a healthcare provider’s prescription.
This shift began in mid-December when the first EUA for at-home testing was issued for the Lucira COVID-19 All-In-One Test Kit (See At-Home COVID-19 Testing Finally Arrives: Laboratory Expert Weighs in on the Implications for Clinical Laboratories). Until that point, COVID-19 specimens could be collected at home but were required to be sent to a clinical laboratory for testing. The Lucira test marked the first COVID-19 test that could be performed completely at home, bypassing the need for clinical laboratories.
Another milestone in COVID-19 testing moving out of the healthcare arena shortly followed. In early December, LabCorp’s Pixel COVID-19 Test Home Collection Kit was granted an EUA that allowed the test to be sold to consumers without requiring a prescription (See FDA Issues EUA for First-Ever Direct-to-Consumer COVID-19 Test, Moving COVID-19 Further From Clinical Laboratories). This development reduced the control that healthcare providers had over COVID-19 testing and offered further flexibility for consumers.
These two traits were finally combined in mid-December when the Ellume COVID-19 Home Test became the first over-the-counter, fully at-home COVID-19 test (See New EUA Makes COVID-19 Testing Available for Patients Without Clinical Laboratories Playing a Role). Ellume has already announced an ambitious rollout of this new test, allowing access to COVID-19 testing that does not require any contact with a healthcare professional and does not utilize clinical laboratories.
3. Secondary Tests, Including Coagulopathy Tests
While COVID-19 testing often brings to mind diagnostic tests such as PCR or antigen testing, there are many other tests that should occur for those who have been tested for COVID-19. As our understanding of COVID-19 and its effects has grown, so too has our understanding of how to test those who have been diagnosed with COVID-19.
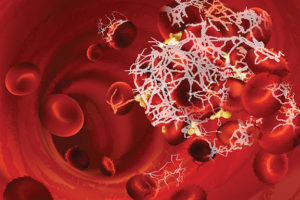
One area of secondary testing for those who were COVID-19 positive was coagulopathy testing. Early in the pandemic, Joshua Hayden, PhD, DABCC, FAACC, Chief of Chemistry for Norton Healthcare and former Assistant Professor of Pathology and Laboratory Medicine at Weill Cornell Medical College told STAT COVID-19 that clinical laboratories should consider testing D-dimers, partial thromboplastin times (PTTs), and fibrinogen on all COVID-19 positive individuals (See Clinical Laboratories May be Overlooking Coagulopathy Tests That Should be Ordered for COVID-19 Positive Patients). COVID-19-associated hypercoagulopathy pathways are better understood now, and research also indicates that testing for antiphospholipid (aPL) antibodies may help to predict the risk of hypercoagulopathy (See University of Michigan Team Delivers Insights Into Hypercoagulopathy With COVID-19).
Frederick (Fritz) Kiechle, MD, PhD, Medical Director at Boca Biolistics and a well-known pathologist, also explained to STAT COVID-19 readers a variety of clinical biomarkers that clinical laboratorians should consider based on each stage of an individual’s disease progression (See Overlooked Clinical Biomarkers Play Important Role in Determining and Predicting COVID-19 Disease Severity).
While additional COVID-19 tests are useful and necessary in measuring disease progression and formulating prognoses, research has also indicated that routine laboratory testing is only supportive once a diagnosis has been made through molecular testing. Research has shown that routine laboratory tests, while often necessary after diagnosis, are not useful in making an initial diagnosis (See Recent Study Concludes That No Routine Laboratory Test Reliably Serves as a Biomarker for COVID-19).

—By Caleb Williams, Editor, COVID-19 STAT
Related Resources:
Lucira COVID-19 All-In-One Test Kit






