New CDC guidelines for COVID-19 vaccine distribution may help clinical laboratories avoid COVID-19-related staffing shortages
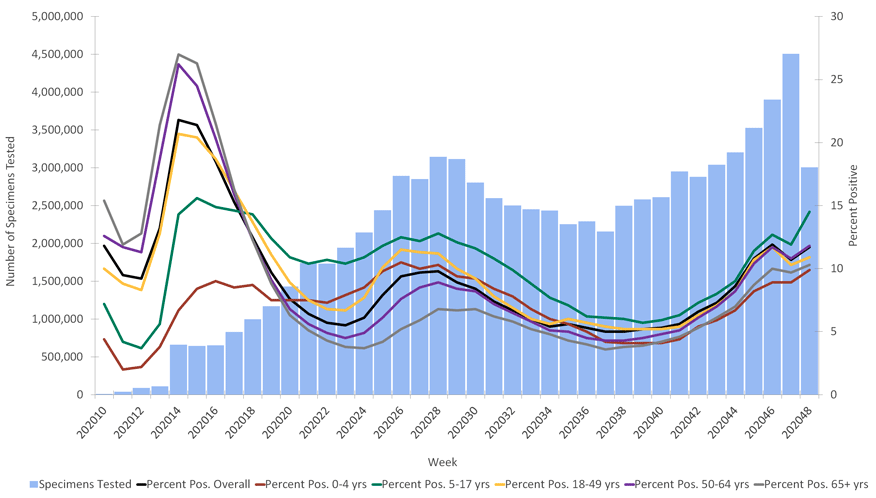
The US Centers for Disease Control and Prevention (CDC) recently said that the COVID-19 pandemic has increased in intensity with more hospitalizations than at any other point during the pandemic to date. “The overall weekly hospitalization rate is at its highest point in the pandemic with steep increases in individuals aged 65 years and older,” states the most recent CDC update (November 28 weekly report).
Clinical laboratories play a vital role in meeting the nation’s needs during this increase in COVID-19 cases, but labs also face stresses. As COVID-19 cases increase, so does the need for testing. More COVID-19 testing contributes to potential supply chain shortages. Adding to the stresses that clinical laboratories face is the potential for decreased staffing during times when medical laboratory professionals are most needed. During spikes in COVID-19 cases, staff are more likely to contract COVID-19 and be quarantined for two weeks. Even staff that do not have COVID-19 may be out for prolonged periods while awaiting COVID-19 test results for symptoms that occur due to seasonal infections such as influenza.
Vaccine Progress May Alleviate Some Pressure on Clinical Laboratories
With COVID-19 cases rising, a reprieve for staffing issues that clinical laboratories face may soon arrive. Two COVID-19 vaccines have completed phase 3 clinical trials while demonstrating high efficacy rates, and emergency use authorization (EUA) applications have been filed for these vaccines. In particular, the Pfizer/BioNTech COVID-19 vaccine recently gained regulatory approval in the United Kingdom, and authorization is expected soon within the United States. Moderna is the second company to apply for EUA.
With the imminent possibility of an authorized COVID-19 vaccine being available in the United States, the CDC’s Advisory Committee on Immunization Practices (ACIP) met Dec. 3, 2020, to determine how limited vaccine supplies should be allocated. In a near-unanimous decision, ACIP recommended that states prioritize healthcare providers, including those “with direct patient contact and thus who are unable to telework, including those who work in inpatient, outpatient, or community settings, who provide services to patients or patients’ family members, or who handle infectious materials.” ACIP also recommended prioritizing vaccine distribution for long-term care facility residents.
‘Handling Infectious Materials’ Factor in COVID-19 Vaccine Distribution
Clinical laboratory professionals would include healthcare providers that “handle infectious materials” and would thus be among those initially prioritized for receiving the COVID-19 vaccine. This development may help clinical laboratories to avoid staffing shortages due to COVID-19 infections and necessary quarantines. Vaccination may also help to prevent the spread of COVID-19 in the workplace.
Advocating for Clinical Laboratory Priorities With State-Level Officials
While ACIP’s recommendations offer the potential for clinical laboratory staff to be vaccinated and avoid workflow disruptions caused by COVID-19, the committee’s recommendations are not binding. States will ultimately be responsible for how they choose to distribute COVID-19 vaccinations. Clinical laboratory leaders may benefit from collaborating with state officials who are responsible for organizing COVID-19 vaccine distribution and ensuring that laboratorians are represented in vaccine rollout plans.
Clinical laboratories should also prepare for adjusting workflows, COVID-19 related sick leaves, and staffing policies for vaccinated staff. The impending availability of a vaccine has been sudden, and the CDC has not yet released recommendations on how to adjust staffing and workflows once healthcare providers have been vaccinated. At least initially, clinical laboratories and other clinical entities may have to prepare for this eventuality themselves.

—By Caleb Williams, Editor, COVID-19 STAT
Related Resources:
Center for Infectious Disease Research and Policy: Update Nov. 30